The Vagus Nerve - What is it?
The Vagus nerve or vagal nerves are the main nerves of the parasympathetic nervous system. They are the 10th of 12 cranial nerves. It contains both motor and sensory functions in afferent (conducting inward or toward something) and efferent (conducting outward or away from something) regards. The vagus nerve does have an effect on several different organ systems and regions of the body.
What is the Function of the Vagus Nerve?
They play an important part in the body’s involuntary sensory and motor functions Including:
Digestion
Heart rate, blood pressure
Respiration
Immune system responses
Mood
Mucal and saliva production
Skin and muscle sensations
Speech
Taste
Urine output
Vagal nerves carry signals from the brain to the corresponding areas of the body listed above to stimulate the basic functions.
A more in depth explanation of the function of the Vagus Nerve:
The origin of cell bodies for the vagus nerve originates from the nucleus ambiguous (location of cell bodies of motor nerves). The nerve fibers from the from the nucleus are efferent, special visceral (ESV) fibers that help to mediate swallowing and phonation (production of speech sound). Fibers originating from the dorsal motor nucleus of X are efferent, general visceral (EGV) fibers that provide involuntary muscle control of organs it innervates; those are cardiac, pulmonary, esophageal and, also, innervation to glands throughout the gastrointestinal tract. The superior ganglion of X provides afferent (conducting towards) general somatic innervation to the external ear and tympanic membrane. The inferior ganglion of X provides afferent general visceral fibers to the carotid and aortic bodies; the efferent fibers of this nerve move to the nucleus tractus solitarius (a cluster of neurons located in the brainstem that acts as the primary sensory relay station for visceral information). The inferior ganglion also provides taste sensations to the pharynx and relays this information to the nucleus tractus solitarius.
Where is the Vagus Nerve Located?
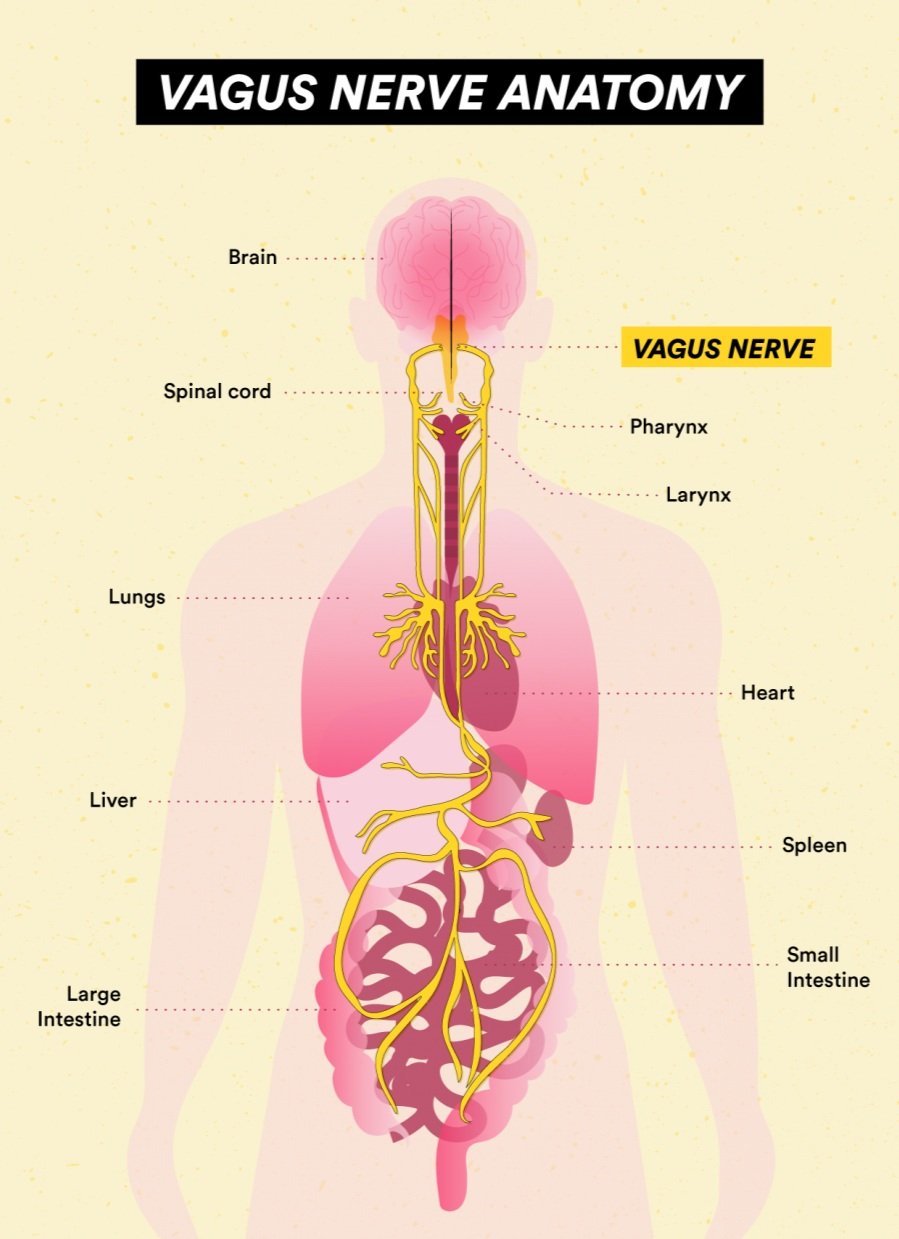
It runs from your brain to the large intestine making it the longest cranial nerve. The left vagal nerve runs down the left side of the body and the right on the right side.
They exit the medulla Oblongata in your lower brainstem, then they connect or pass through the following:
Neck, between the carotid artery and Jugular vein
Chest
Heart
Lungs
Abdomen and digestive tract
*Note on the diagram: This is a general idea of where the vagus nerve, there are branches off of the main stem of the nerve into the tissues
The vagal nerve originates in the medulla oblongata and exits the skull through the jugular foramen. From there, there are two ganglia on the vagus nerve (Superior and inferior) as it exits the jugular foramen, the spinal accessory nerve joins the vagus nerve just below the inferior ganglion. It continues to travel inferiorly (downward) within the carotid shealth. The right vagus nerve travels anteriorly (in the front) to the subclavian artery and posteriorly to the innominate artery (the first branch of the aorta that carries oxygenated blood to the head, neck and right arm), then making it descent into the thoracic cavity to traveling to the right of the trachea and posterior (behind) the hilum (a depression in an organ where the blood vessels, nerves and ducts enter or exit) on the right, now moving medially to form the esophageal plexus with the left vagus nerve, which travels anteriorly to the subclavian artery and enters the thoracic cavity wedged between the left common carotid and the subclavian arteries. It makes its descent then goes posteriorly to the phrenic nerve (the nerve that runs from the spinal cord and the diaphragm) and posteriorly to the left lung, then it travels medially to the towards the esophagus forming the esophageal plexus with the right nerve.
What are each of the Vagus Nerve branches?
The left and right vagal nerves join at the esophageal hiatus to form the vagal trunk where the esophagus passes into your belly. The vagal trunk includes an anterior and posterior gastric nerve that goes to the abdomen.
A more in-depth explanation of the branches:
There are 4 branches of the neck: the pharyngeal, superior laryngeal nerve, the recurrent laryngeal nerve and the superior cardiac nerve
Pharyngeal branch - The pharyngeal nerve branches arise from the inferior ganglion of vagus nerve, it contains sensory and motor fibers. These fibers form the pharyngeal plexus–branches of this plexus innervate the pharyngeal and palate muscles, excluding the tensor palatine muscle); the pharyngeal plexus also supplies the innervation to the intracarotid plexus which mediates information from the carotid body
Superior laryngeal nerve - The superior laryngeal nerve travels between the external and internal carotid arteries; the nerve divides into internal and external branches near the level of the hyoid (The horseshoe bone below the jaw – Adams apple – and above the thyroid cartilage). The internal laryngeal nerve goes through the thyrohyoid membrane(a fibroelastic membrane connecting the thyroid cartilage and hyoid bone), entering the larynx. The external portion travels distally (away from the midline) with the superior thyroid vessels. The external portion supplies the cricothyroid muscle (key muscle in involved in voice production), whereas the internal branch supplies the mucosa superior to the glottis (the opening between the vocal folds in the larynx).
Recurrent laryngeal nerve - The right recurrent laryngeal nerve fibers branch from the vagus nerve near the right subclavian artery, traveling superiorly to enter the larynx between the cricopharyngeal muscle and the esophagus. The left recurrent laryngeal nerve then loops around the aortic arch distal to the ligamentum arteriosus and enters the larynx. All of the laryngeal musculatures receive supply via the recurrent laryngeal nerve except for the cricothyroid muscle (supplied by the laryngeal nerve)
Superior Cardiac Nerve - While the vagus nerve is within the carotid sheath, it gives off the superior cardiac nerve, is associated with parasympathetic fibers, and travels to the heart
Anterior and posterior bronchial branches - The vagus nerve gives off anterior and posterior bronchial branches, the anterior branches along the anterior lung, forming the anterior pulmonary plexus. In contrast, the posterior branches form the posterior pulmonary plexus
Esophageal branches - Esophageal branches of the vagus nerve are anterior and posterior and form the esophageal plexus. The left vagus is anterior to the esophagus; the right vagus is posterior
Gastric and celiac branches - Gastric branches supply the stomach; celiac branches (mainly derived from the right vagus nerve) supply the pancreas, spleen, kidneys, adrenals, and small intestine
Understanding the signs of Vagus Nerve Dysregulation?
If you haven’t caught yet, the Vagus Nerve has its hands in most of our basic day-to-day functions which makes understanding the signs of dysregulation so important.
First let’s gain an understanding of the word dysregulation.
dysregulation (the Merriam-Webster definition)noundys·reg·u·la·tionimpairment of a physiological regulatory mechanism (as that governing metabolism, immune response, or organ function).Basically meaning anytime the mechanism is NOT functioning properly or optimially there is some level of dyregulation.
Signs & Symptoms of Vagus Nerve Dysregulation - these will vary based on the affected organ and this is not a comprehensive list.
Abdominal pain and bloating
Acid Reflux
Changes to heart rate, blood pressure or blood sugar
Difficulty swallowing or loss of gag reflex
Dizziness or fainting
Hoarseness, wheezing or loss of voice
Loss of appetite, feeling full quickly or unexplained weight loss
Nausea and vomiting
heart palpitation
changes in bowel movements
anxiety/depression/irritability,
mood fluctuations
insomnia
High Cortisol levels
What is Vagus Nerve Regulation?
Regulating the vagus nerve involves doing things that interact with the vagus nerve itself. These things include but are not limited to:
Breath work – deep breathing specifically- one of the easiest ways to stimulate the vagus. Nerve is by harnessing your breath, it helps to slow down the heart rate, lower blood pressure. Decreases anxiety and stress responses. Diaphragmatic breathing is the best kind of vagus nerve stimulation (breathing deep into your belly, make sure your exhales are longer than the inhales. Remember I thought the nose out through the mouth) There are several kinds of breathe work such as box breathing (Breathe in for 4 seconds, hold for 4 seconds, exhale for 4 seconds), the Wim Hof Breathing Technique, 4-7-8 method (Breathe in for 4, hold for 7, exhale for 8). Holotropic breathing (deep and rapid breathing).
Meditation
Sound – Sounds such as humming, singing, gargling water, om-ing, laughing are all great and easy ways to start regulating the vagus nerve. These increase heart variability and vagal tone; heart rate variability is the differences in the duration BEWTEEN heartbeats. High heart rate variability is typically linked to better vagal tone. When you hum, sing or gargle you are activating the muscles in the throat that are linked to the vagus nerve thus stimulating vagal stimulation
Gratitude Journaling - in the morning or evening write down 3 things that you are grateful for. These things can be as little as the breathe in your lungs to as big as the house you live in. Create a repetitive routine at a cadence that feels right to you.
Rubbing behind the ears is a direct contact spot for the vagus nerve that helps to regulate the nerve directly. There are also various positional holds that will be available in the Facebook Group soon that help to regulate the vagus nerve too.
Cold exposure – Your body triggers the physiological response called the mammalian diving reflex/response when exposed to cold water. This response slows the heart rate which in turns helps to keep you calm. Research has shown this to be an excellent way to improve heart rate variability and vagal tone.
Ways to practice cold exposure include:
Cold showers
Cold plunge
Submerge your face in a bowl of ice water
Holding an ice pack to your neck
Physical Exercise- Interval and endurance training are great for activating the vagus nerve.
Massage Therapy – research has shown that massage to the head and neck can stimulate the vagal sensory neurons and activate the parasympathetic system which triggers the rest and digest mode
Connecting with nature - This allows your body to reconnect with the nature frequencies outside of your day-to-day happenings. Taking your shoes off and letting your feet connect with grass or dirt directly allows a direct connection to the Earth’s natural frequencies. Taking a walk in the woods, hiking, swimming in natural bodies of water, sitting under the sun are all excellent ways to connect with nature. These activities increase your vagal tone.